Transoral Robotic Surgery for Obstructive Sleep Apnoea
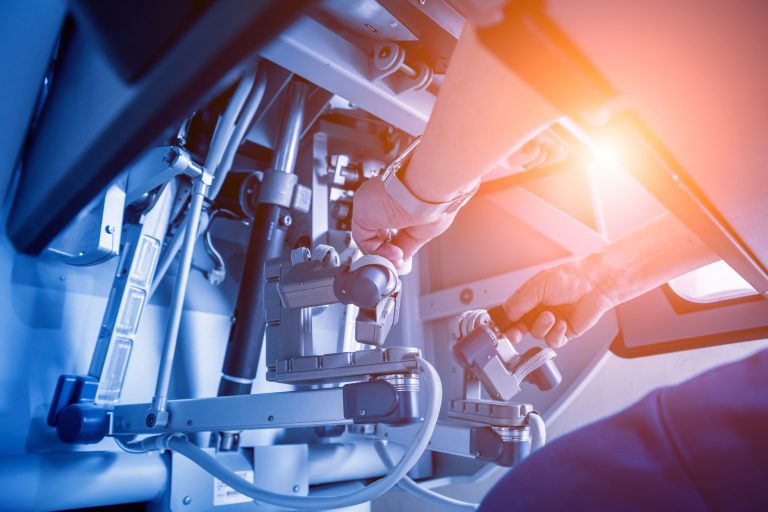
Transoral Robotic Surgery (TORS) is a minimally invasive surgical technique that uses a robotic system to access, visualise and operate in the oral cavity and throat. I use the DaVinci© Robotic system in my practice.
I offer transoral robotic surgery of the tongue base in carefully selected patients with obstructive sleep apnoea (OSA) who cannot tolerate or want an alternative option to long-term CPAP (continuous positive airway pressure) therapy. In many such patients the tongue base is a big contributor to their mechanism of apnoea.
The aim of the operation is cut out the central bulk at the back of the tongue to clear a pathway to the voice box entrance.
Who is suitable for TORS?
Here are some indications that I use to guide decision making:
You should have Moderate to Severe Obstructive Sleep Apnoea.
Your BMI (body mass index) should ideally be less than 35. The lower it is the greater the chance of success.
Your sleep nasal endoscopy (SNE) would have determined a favourable pattern of obstruction that predicts a successful outcome. These could include: a large tongue base, large lingual tonsils, a tongue base that collapses into the airway or one that causes the epiglottis (the lid of cartilage covering your voice box) to flop back to shut the voice box.
My decision to offer TORS will also be influenced by other anatomical factors such as good mouth opening and the need to perform other operations where obstruction occurs at multiple levels in the air passages.
Potential complications
Whilst the procedure is minimally invasive, requiring no external incisions, there are some potential risks associated with it.
You will be nursed in a high dependency unit with close monitoring during the first night post-op. You will need to stay in the hospital for a few days afterwards to acclimatise to pain and swallow.
The risk of post operative bleeding that warrants a return to theatre is less than 1 in 100.
Any loose teeth, caps or crowns may become dislodged.
Swelling in the oral cavity and throat area is common after surgery. This is usually temporary, but significant swelling may affect breathing and swallowing that may require medication and close monitoring.
Unfortunately, the procedure can be very painful. We will provide you with an effective pain management plan to alleviate the discomfort during the recovery period.
You will also be put on a course of antibiotics and antiseptic gargles to reduce infection risk.
Your swallow will unfortunately be troublesome and painful postoperatively, but recovers within a week or so. Very rarely, there is a small risk of food or fluid entering the airway (aspiration) after surgery. This will usually normalise with dietary modification and speech and swallow therapy.
A small number of patients also report a change in taste or the feeling of a foreign body in the back of the throat. These resolve in most patients after a few months.
As the tissues heal, they can form a scar band that may impact the flexibility and function of the throat muscles. This may require an additional surgical procedure to correct. This is extremely rare.
The surgery is usually successful and most people will have at least an improvement of the severity of their OSA.
Happily, approximately 75% of suitable patients in my hands do not require CPAP once healed.
