Functional endoscopic sinus surgery (FESS)
Functional endoscopic sinus surgery (FESS) is an integral part of my practice for managing both chronic and in some cases acute conditions that block the sinuses and the nasal cavities. I will typically recommend surgery when tablet and spray form medication has not effectively managed your symptoms and when cross sectional imaging such as CT has demonstrated disease within/ affecting the sinuses.
Common conditions that require surgical intervention with FESS
Chronic Sinusitis. Chronic sinusitis is characterized by persistent inflammation of the various sinus and nasal cavities, leading to symptoms that include nasal block/ congestion, facial pain or pressure, postnasal drip, and a reduced sense of smell. When symptoms persist despite medical therapy, I may recommend FESS as part of a surgical plan to open up the sinuses’ outflow tracts.
Nasal Polyps. Nasal polyps are non-cancerous growths of sinus and nasal lining that often develop in the sinuses and grow out into the nasal cavity. They can obstruct normal mucous drainage as well as cause a physical block to nose breathing. Polyps can grow very large and, in some patients, may even hang out of the nose! Larger polyps cause nasal block/ congestion, recurrent sinusitis, and tellingly, an impaired sense of smell.
In patients who also suffer from nasal allergy, asthma and/ or who are insensitive to aspirin type medication, polyps are particularly resistant to medical management.
FESS will be used to remove these polyps, to not only relieve symptoms in the short term, but to aid medication delivery into the open sinus cavities and prevent recurrence in the long term.
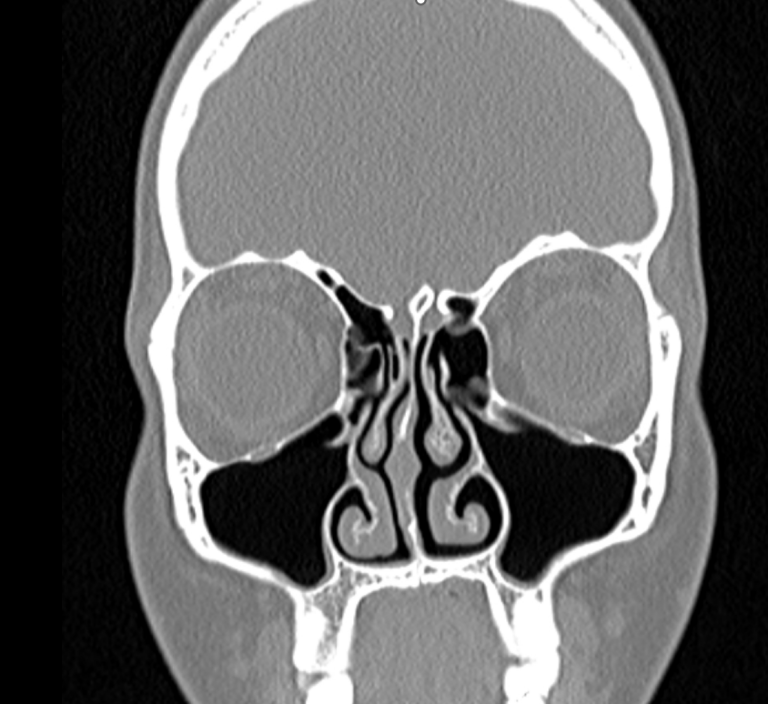
Structural Abnormalities. People may be born with certain anatomical abnormalities within the nose and sinuses that can impede proper sinus drainage and ventilation; these may ultimately contribute to recurrent or chronic sinusitis. They include a deviated septum, concha bullosa (which refers to a ballooned middle turbinate bone that lies in front of the common sinus drainage outflow passage), or particularly narrow sinus openings. I use FESS to address these anatomical issues to open up the sinuses’ outflow pathways.
Recurrent Acute Sinusitis. A number of my patients have experienced recurrent episodes of acute sinusitis despite prolonged, maximum medical treatment. This has usually been associated with one/ more of the underlying structural abnormalities noted above. If so, FESS may be beneficial to remedy the acute infection and to prevent further infections.
Complications of Sinusitis. Untreated severe or acute on chronic sinus infections can sometimes lead to serious or life-threatening complications such as orbital cellulitis (infection of the tissues around the eye), abscess formation, or even intracranial infection. In such cases an emergency FESS procedure may be required to drain infected material in order to buy time until the intravenous antibiotics and other medication starts to eradicate the infection.
Preparation for Surgery
I usually perform FESS as a day surgical procedure.
Your medication regime for your specific condition will have been optimised. This will not only help minimise complications during the operation but will also speed up post operative recovery.
The hospital will contact you to perform a comprehensive preassessment and may recommend adjustments to your current medications, particularly blood thinners, to minimize the risk of bleeding during surgery.
The Surgery
Endoscopic sinus surgery will be performed under general anaesthesia. The procedure will be performed through the nostrils using a small rod like camera to provide a magnified view of the nasal cavity and sinus anatomy. I will utilise specialised instruments such as a microdebrider to remove diseased tissue, polyps and bone to open up the sinuses. It may be necessary to perform a septoplasty to make space for the instruments as well as to relieve nasal obstruction in its own right.
The surgery usually lasts between 1 to 1.5 hours but will vary depending on complexity or if additional procedures like a septoplasty or inferior turbinate reduction need to be performed.
Postoperative Care
I usually place self-dissolving nasal packing into the sinuses to support healing and capture and minimize postoperative bleeding. I will prescribe you a course of tablet antibiotic and appropriate pain medication to prevent infection and alleviate discomfort during the first week of recovery. I will also prescribe decongestant nasal drops and an antibiotic nasal cream.
You may get a small, self-limiting trickle of blood from the nose for a few days afterwards. This is normal. You will also feel very blocked in the nose due to the packing material.
I recommend you take 2 weeks off work (although you may be able to work from home if that is an option). During this period, please abstain from strenuous exercise or heavy lifting and avoid hot or spicy food and beverage to reduce the risk of bleeding.
I will schedule a follow-up appointment about 2 weeks after your operation to remove the residual nasal packing and to ensure healing is progressing well.
Potential Risks and Complications
Here is a list of specific complications to be aware of. They are rare, but if you are concerned, I am happy to be contacted, out of hours if necessary, to guide further management.
Although a small amount of blood from the nose can be expected, heavy bleeding in the day or two after the operation is more worrying. If this occurs then you will need to visit your local accident and emergency department in the first instance.
Bleeding after a week or so is usually related to an infection; at this stage you may also have a fever or pus like discharge from the nose. I routinely give my patients a course of antibiotic post op to prevent a secondary sinus infection.
Because the sinuses are located between the eye cavities (orbits) and the frontal brain cavity, inadvertent instrumentation into these areas may cause damage to their contents. These serious complications are extremely rare with modern visualisation and surgical technique (less than 1:3000 in the literature, although I personally haven’t experienced any of these complications!).
Some patients have a reduced sense of smell after the operation if the smell nerves (olfactory-nerves) have been injured. However, for most people, their sense of smell usually improves after the operation because a pathway from the front of the nose to the smell area opens up, allowing free flow of odorant chemicals.
Occasionally, I may have to offer a revision operation in cases where the disease recurs or if unusual scarring has re-sealed the sinuses.
In general though, endoscopic sinus surgery offers a safe and effective solution for a variety of protracted sinus disorders, providing relief and improved quality of life for my patients.
